What are the HIPAA Training Requirements?
HIPAA, the Health Insurance Portability and Accountability Act, outlines certain requirements to ensure the privacy and security of protected health information (PHI). Among these requirements is the need for training healthcare personnel on HIPAA’s privacy and security rules.
HIPAA Training Requirements:
Initial Training: New employees or staff members should receive HIPAA training shortly after being hired. This helps them understand the importance of protecting PHI and their responsibilities regarding the same.
Annual Training: While HIPAA doesn’t specify an exact frequency for training, many organizations conduct annual refresher courses to ensure their staff stays updated on changes in policies, procedures, or regulations.
Training Content: Training programs must cover the organization’s privacy and security policies, procedures, and practices. This includes how to handle, store, and transmit PHI securely.
Specialized Training: Different roles might require different levels of training. For example, IT professionals might need detailed training on encryption and securing digital PHI, while administrative staff might focus more on privacy practices.
Documentation: Organizations must keep records of their training programs, including who was trained, the date, and the content of the training. This documentation is essential for compliance checks and potential audits.
Response to Changes: Whenever there are significant modifications to the privacy rule, security rule, or other HIPAA-related procedures, affected employees must be re-trained accordingly.
Training Format: The format (online, in-person, workshops, etc.) isn’t strictly defined by HIPAA. Organizations can choose a training method that suits their needs, provided it effectively educates employees.
Security Reminders: Beyond formal training sessions, HIPAA’s security rule recommends periodic security reminders. These can be in the form of emails, newsletters, or short meetings.
How Often is HIPAA Training Required?
Under HIPAA (Health Insurance Portability and Accountability Act) regulations, there isn’t a specific frequency mandated for training employees. However, the Department of Health and Human Services (HHS) recommends that training should be provided for all new hires and at least annually for existing staff.
Additionally, it’s advisable to conduct HIPAA training whenever there are significant changes in policies, procedures, or regulations that affect how protected health information (PHI) is handled. This ensures that all personnel remain updated on their responsibilities and the latest compliance requirements.
What Should be Included in a HIPAA Training Course?
A HIPAA training course should comprehensively educate participants about the Health Insurance Portability and Accountability Act’s rules and how they apply to the daily operations of healthcare and affiliated businesses. Here are essential components that should be included in a HIPAA training course:
Introduction to HIPAA:
The Health Insurance Portability and Accountability Act (HIPAA) was instituted in 1996. Initially created to enhance healthcare access and protect the health insurance rights of workers, it later expanded its focus to include data protection.
Historical Background and Purpose of HIPAA:
HIPAA’s enactment was groundbreaking. Beyond improving healthcare accessibility, it set out to ensure that patient information would be kept confidential and secure across healthcare environments.
The Importance of Patient Privacy and Security:
In healthcare, confidentiality isn’t just ethical—it’s crucial. Protecting patient details ensures trust in the healthcare system and prevents potential misuse of sensitive information.
Definitions:
- Protected Health Information (PHI): Refers to any personal health information that can identify an individual and is shared or used within a healthcare context.
- Electronic Protected Health Information (ePHI): This is PHI that’s stored or transmitted electronically.
- Covered Entities (CE): These are healthcare providers, health plans, and health clearinghouses involved in the transmission of health information
- Business Associates (BA): Third-party entities that handle or have access to PHI due to their work with a covered entity.
HIPAA Privacy Rule:
This rule safeguards patients’ medical records and other personal health information.
- Basic Principles: Ensures that an individual’s health information is properly protected while allowing the necessary flow of health information to provide quality healthcare.
- Types of Information Protected: Any information that can identify an individual, such as name, address, birth date, etc., and is transmitted or maintained in any form.
- Permitted Uses and Disclosures: For treatment, payment, and health operations unless expressly told otherwise by the patient.
- Patient Rights: Patients have rights to their health information, including rights to inspect, amend, and know who has accessed their records.
HIPAA Security Rule:
This rule sets standards to safeguard ePHI.
- Administrative, Physical, and Technical Safeguards: Processes, physical barriers, and technology controls used to protect ePHI.
- Security Risk Assessments: Regular evaluations to determine vulnerabilities in the protection of ePHI.
- Implementation of Security Measures: Employing defenses against vulnerabilities.
- Use of Encryption: Ensuring ePHI isn’t accessible during transit or at rest.
Breach Notification Rule:
Dictates the protocol for when a breach of PHI occurs.
- Definitions of Breaches: Unauthorized use or disclosure of PHI.
- Reporting Requirements: Covered entities must promptly notify affected individuals and, in some cases, the media and the Secretary of Health and Human Services.
- Potential Penalties: These can range from monetary fines to criminal charges, depending on the nature of the violation.
Enforcement and Penalties:
- Enforcement Agencies: The Office for Civil Rights primarily oversees compliance.
- Different Tiers of Penalties: Fines range based on the level of perceived negligence.
- Real-life Cases: Over the years, multiple organizations have faced penalties for not adhering to HIPAA rules, from small clinics to large hospital networks.
[Also Read: Understanding HIPAA Privacy Rule: The Three Fundamental Rules to Keep in Mind]
HIPAA and Technology
Proper Use: Guidance on the acceptable use of email, social media, and mobiles.
Safeguarding ePHI: Protecting ePHI within electronic health records.
Cloud Storage: Evaluating and choosing secure cloud storage solutions.
Best Practices:
- Policies and Procedures: Creating standard operating procedures for handling PHI.
- Employee Training: Regular HIPAA education for all staff.
- Audits and Assessments: Periodic checks to ensure compliance.
Special Considerations:
- Working with BAs: Ensuring third-party vendors also comply with HIPAA.
- Specific Roles: Tailoring training and guidelines for roles like IT personnel, nurses, and office staff.
HIPAA in the Modern Context:
- Recent Updates: As healthcare and technology evolve, so does HIPAA. It’s essential to stay updated on any changes.
- Emerging Challenges: With innovations like telehealth and wearables, new challenges arise that require continuous adaptation.
Interactive Scenarios and Case Studies:
- Practical Examples: Test understanding through real-life scenarios.
- Risk Discussions: Delve deep into potential risks and strategies to handle them.
Conclusion and Resources:
- Recap: A summary of HIPAA’s principles and their importance.
- Further Reading: It’s imperative to be proactive, seeking out resources to ensure ongoing compliance and understanding of HIPAA regulations.
HIPAA Training Requirements
Employees:
All employees in healthcare settings must receive training on HIPAA regulations to understand the importance of protecting patient information. This training introduces the basics of HIPAA, the concepts of PHI (Protected Health Information), and the responsibilities each employee has in safeguarding it.
Refresher Training:
Periodic training is designed to update and remind employees of their HIPAA responsibilities. It’s essential to keep staff updated on any changes in policies, procedures, or regulations and to ensure continued compliance.
Nurses:
Focused on the specific needs and roles of nurses in patient care. Training covers how to handle PHI in clinical settings, communicate with patients and families, and collaborate with other healthcare providers while ensuring patient privacy.
IT Professionals:
Tailored for those who manage electronic health records, databases, and other technical systems. It emphasizes the importance of securing ePHI, implementing technical safeguards, encryption, and managing potential cybersecurity threats.
Medical Office Staff:
Targets administrative roles in healthcare, like receptionists and office managers. The training covers topics such as patient record management, appointment scheduling, and ensuring the confidentiality of verbal and written communications.
Business Associates:
Business associates are third-party entities that have access to PHI due to their work with healthcare organizations. They need training to understand their responsibilities under HIPAA, especially when handling, transmitting, or storing PHI.
HIPAA Compliance Training for Business Associates:
A more in-depth training that not only covers the basics of HIPAA but also the specifics of ensuring compliance in their operations. Topics might include performing risk assessments, drafting Business Associate Agreements (BAAs), and implementing robust data protection measures.
HIPAA Training Benefits
The benefits of HIPAA (Health Insurance Portability and Accountability Act) training are numerous, both for the healthcare organizations and the patients they serve. Here are some key advantages:
Enhanced Patient Trust: Patients are more likely to trust healthcare organizations that prioritize the confidentiality and security of their personal health information. Training ensures employees handle such information properly, fostering trust.
Reduction in Data Breaches: Properly trained staff are less likely to make errors that could lead to breaches of sensitive data, thereby preventing costly and damaging breaches.
Regulatory Compliance: Regular HIPAA training ensures that healthcare organizations remain compliant with federal regulations, helping them avoid hefty fines and legal complications.
Improved Staff Confidence: When employees understand the rules and know how to apply them in their daily tasks, they can work with greater confidence and efficiency.
Standardization of Procedures: HIPAA training offers a standardized approach to handling patient data, ensuring consistency throughout the organization.
Risk Management: By training employees on the potential risks associated with mishandling PHI (Protected Health Information), organizations can more effectively manage and mitigate these risks.
Efficient Response to Incidents: In the event of a potential data breach or other incidents, trained employees will know the appropriate steps to take, ensuring a swift and effective response.
Adaptability to Technological Changes: With the healthcare industry’s ongoing digital transformation, it’s essential that staff are trained in how to handle electronic PHI (ePHI) and are aware of the associated risks and safeguards.
Enhanced Reputation: Organizations that prioritize and invest in training demonstrate a commitment to patient privacy and data security, bolstering their reputation in the healthcare industry.
Informed Decision Making: Training helps staff understand the implications of their actions concerning PHI. This knowledge aids in making informed decisions, especially in complex or ambiguous situations.
Cost Savings: While there’s an upfront cost to training, the potential savings from avoiding fines, litigation, and damage to reputation can far outweigh the initial investment.
In summary, HIPAA training is not just a regulatory requirement but offers tangible benefits to healthcare organizations, promoting a culture of data privacy, security, and trust.
FAQ
What is HIPAA training?
HIPAA training educates healthcare professionals and associated staff on the Health Insurance Portability and Accountability Act’s regulations, ensuring the protection of patient health information.
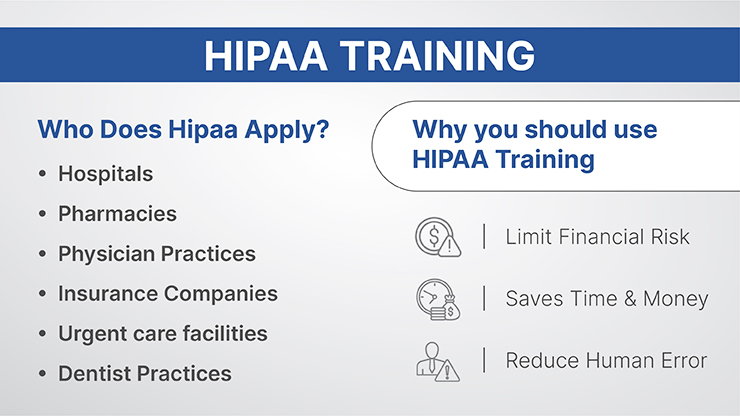
Who needs to undergo HIPAA training?
All members of a healthcare organization, including doctors, nurses, administrative staff, IT professionals, and any third-party business associates who handle protected health information (PHI), should undergo HIPAA training.
How often is HIPAA training required?
While the exact frequency isn’t specified by HIPAA, it’s generally recommended for new hires and at least annually for existing staff. Training should also occur when significant changes to policies or regulations take place.
What topics are covered in a typical HIPAA training session
Training sessions usually cover the HIPAA Privacy Rule, Security Rule, the definition of PHI, the proper handling and storage of PHI, breach notification procedures, and penalties for non-compliance
Can HIPAA training be done online?
Yes, online HIPAA training is widely available and can be a flexible and convenient option for many organizations. It’s crucial to ensure that the online training platform covers all necessary topics comprehensively.
What are the consequences of not completing HIPAA training?
Non-compliance can result in severe penalties, including substantial fines and potential legal actions. Besides, it may also lead to unintended data breaches, harming the organization’s reputation.
Is there a certification process after HIPAA training?
While there’s no official certification for HIPAA training, many organizations provide certificates of completion to participants. These can serve as proof of training for audits and internal records.
How does HIPAA training differ for IT professionals and medical staff?
While the foundational principles remain the same, training for IT professionals will place more emphasis on electronic data protection, cybersecurity, and technical safeguards. Medical staff training will focus more on patient interactions, clinical data handling, and communication.
What should I do if I believe there’s been a HIPAA violation in my organization?
Organizations should have a clear process in place for reporting and addressing potential HIPAA violations. If you suspect a breach, you should immediately report it to your supervisor or designated compliance officer.
How do I stay updated on changes to HIPAA regulations?
Regular refresher training sessions, subscribing to healthcare law newsletters, and being part of professional healthcare organizations can help you stay informed about updates or changes to HIPAA regulations.